Terman, Ph.D., M.D., is a
psychiatrist and bioethicist. He lives in
Sausalito. Steinberg, M.D., is a
hospice and palliative medicine specialist,
bioethicist and nursing home and hospice
medical director in Oceanside. The opinions
expressed are those of the authors, not the
organizations with which they are
associated.
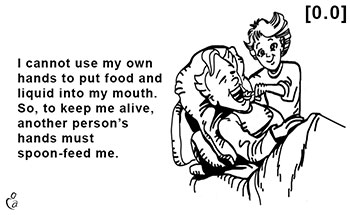
No one doubts the importance of
completing living wills — especially for
advanced dementia — a cruel disease that
most people dread since it can cause
prolonged dying with severe, irreversible
suffering as it imposes huge burdens on
loved ones. But by themselves, living wills
will not be adequate if your future
physician refuses to honor its requests. A
recommended request is: “Cease putting food
and fluid into my mouth if I reach a
specific condition.” Honoring this request
can prevent being forced to endure years of
suffering since you will not need to wait to
die from a heart attack, or untreated
infection such as pneumonia. After you no
longer can feed yourself, the only legal,
peaceful and effective intervention may be
to cease assisted feeding and hydrating by
another’s hand. This challenging and
controversial intervention raises questions
for your physician, and for you.
Is your physician’s refusal to honor your
wishes good or bad? “Good” means in your
“best interest” such as preventing premature
dying. “Bad” means forcing you to endure
prolonged, and likely increased, suffering
with little or no benefit.
Are physicians’ actions well-meaning or
selfish? “Selfish” means refusal benefits
your physician as it harms you. Physicians’
hubris leads to their desiring that their
actions are viewed favorably — while you
suffer longer, and more. Many physicians
want to view themselves as heroes who
sustained your life. But the ethical
position of the American Medical Association
is clear: “The social commitment of the
physician is to sustain life and relieve
suffering. Where the performance of one duty
conflicts with the other, the preferences of
the patient should prevail.”
A comprehensive question for physicians
to ask: Are their actions legal, ethical and
respectful? You have a claim right to
self-determination (what happens to your
body) and to avoid suffering. Claim rights
impose a duty on others to act by honoring
your rights, so ... physicians should
attempt to reduce your suffering and
physicians should not violate your bodily
integrity. This includes assisted oral
feeding and hydrating — if you previously
refused it. In addition to being unethical,
force feeding may be illegal since battery
is a crime. Yet some physicians argue they
must consider all available information,
strive to do no harm and maximize what they
feel is your benefit. Hence, your living
will’s future success depends on your
resolving common conflicts during advance
care planning.
Some questions for you: Do you prefer
fast and easy living wills that ask you only
to check a few boxes before signing? Do you
consider your task complete once you clearly
expressed your wishes? Is your living will
specific enough to avoid conflict? Is it
comprehensive so you don’t suffer from
omitted conditions? Does it strive to be
“clear and convincing” — the highest
evidence standard in civil law? Will you
record a persuasive video on which you state
what you want, and explain why?
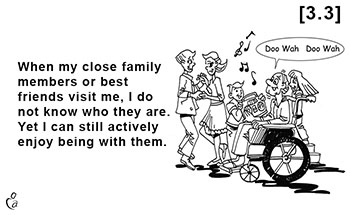
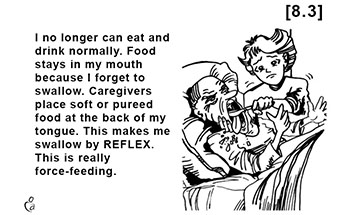
Even the above amount of effort may not
be successful. A large, influential
physician organization,
The Society for Post-Acute and Long-Term
Care Medicine, recommends not honoring
requests to stop assisted feeding until you
manifest behavior it interprets as either
refusal or distress. Also, physicians and
others can allege you changed your mind
based on observing you open your mouth and
swallow what others put in. But your
apparently cooperative behavior may result
from reflex or habit, after dementia has
caused you to forget your critically
important life values — to avoid suffering
and imposing burdens on others.
Advance care planning must lay the
groundwork to persuade future physicians to
honor your end-of-life wishes. Living wills
can include cogent arguments that cite
clinical literature and case law to compel
your physician to respond — especially if
conflicts escalate to court. Among several
recommended strategies, here are two.
Insist no one can claim you changed your
mind to want spoon feeding — unless two
experts qualified in the fields of dementia,
capacity and assisted feeding so testify
within a reasonable degree of medical
certainty.
Store your printed forms and videos in an
electronic registry so physicians and EMTs
can expeditiously retrieve the current
versions.
Admittedly, there is no proof (yet) that
adding recommended strategies will increase
your chance of success. (The reason: it will
take years to gather enough data for those
who completed advance care planning to
eventually encounter conflicts.)
So can you trust doctors to honor your
end-of-life wishes? Are you kidding? Current
experience leads to this recommendation: Do
not kid around. Put in the required time and
effort to give yourself the best chance of
experiencing a peaceful and timely dying.
Terman, Ph.D., M.D., is a psychiatrist
and bioethicist. He lives in Sausalito.
Steinberg, M.D., is a hospice and palliative
medicine specialist, bioethicist and nursing
home and hospice medical director in
Oceanside. The opinions expressed are those
of the authors, not the organizations with
which they are associated.